- Nov 7, 2025
From Fields to the Brain: The Connections Between Pesticides and Epilepsy
- Faisal Jahangiri
- neuromonitoring, neurophysiology, Blogs, EEG
- 0 comments
How is it that something like pesticides can impact human health deeply enough to lead to seizures?
It is well known that different chemicals can produce negative effects on the chemistry of the human brain. After all, people are surrounded by environmental toxins from the air they breathe to the food they eat. Pesticides are specifically something of focus because they are a pollutant on both the agricultural and individual levels, one of the many categories of chemicals to be cautious of. They can be rather easily spread through touch, consumption, and inhalation. The specific relation to epilepsy is one that should be studied more than it has been, especially since epilepsy is one of the most common global neurological diseases. Additionally, there are certain populations of people that are affected most by pesticides, possibly even on a daily basis of contact. The main group of these populations is those working in agricultural fields. Such populations are also in low-income areas, worsening the effects of the issue.
Epilepsy
Epilepsy is a seizure disorder that impacts people of a variety of backgrounds and characteristics. This includes children and elderly patients alike, which makes epilepsy a widespread issue. Specifically, it is diagnosed in patients who have two or more seizures over the course of a day. This often comes with complexity since the seizures could be seemingly unprovoked. Some of the possible symptoms include muscle stiffness, staring off, loss of consciousness, and psychological changes. For patients with epilepsy, there is some consistency of how the seizures present each time.
Pesticides
There are several classes of pesticides, and each of these has different impacts in relation to epilepsy. Some examples of pesticides are organophosphates, parathion, carbaryl, lindane, strychnine, carbamates, organochlorine, chlorpyrifos, and DDT. DDT is a well-known one as it had a history of wide negative impacts on health before it was banned in many places.
Mechanisms of Pesticides on Seizures
There have been several recent findings on the relationship between pesticides and epilepsy. A paper published in 2012 focused broadly on the chemical toxins that may cause seizures (Jett, 2012). In 2018, there was a paper about the mechanisms by which pesticides can lead to epilepsy, and it included other associations as well (Requena et al., 2018).
One of the major mechanisms by which pesticides can lead to seizures is through GABA receptor inhibition. GABA is an important inhibitory neurotransmitter in the brain which means that it can block nerve impulses. When the GABA receptor is inhibited, this leads to the opposite effect, and there is overstimulation in the brain, making it easier to have a seizure. Lindane is one of the main pesticides known to follow this mechanism.
Another mechanism is the hyperstimulation of cholinergic receptors. Cholinergic receptors use acetylcholine as the ligand that binds to it. The relation to epilepsy and seizures lies in how the acetylcholine is responsible for muscle contraction, and there are effects that lead into the brain as well. An example of a pesticide that contributes in this way is organophosphorus and its related chemicals.
The next mechanism to discuss is related to the previous one since it relates to acetylcholine. Basically, with the inhibition of acetylcholinesterase, or the enzyme that breaks down acetylcholine, there is that overstimulation from acetylcholine going to its receptors and causing imbalances.
A fourth mechanism exists as well, and this is about ion flow. Specifically in voltage-gated sodium channels, the sodium ions flowing through have consequences on the nerve impulses that are sent through the brain. Seizures are particularly affected by the number of impulses at a given time, with hyperactivity being characteristic of most, if not all, seizures.
Different Categories of the Pesticides
Epileptogenic pesticides that can induce seizures are only a part of the larger repertoire of pesticides. This includes chlordimeform, chlorpyrifos, amitraz, endosulfan, and lindane. Of these, lindane was specifically related to the GABA receptor inhibition mechanism of inducing seizures.
The other pesticides that do not have as much research linking them to epilepsy or seizures include mepiquat, fipronil, lufenuron, lambda-cyhalothrin, and glufosinate. Each of these pesticides work in different ways on plants, so it makes sense that there are varying impacts on humans.
Affected Parts of the Brain
In general, there are a variety of seizures that could occur based on what the causes are or other factors. Absence seizures, often seen as if the person is staring off, are much different from tonic-clonic seizures, which shows up as cycles of stiffness and jerking.
Seizures related to pesticide exposure could occur in various places in the brain as each individual has different experiences. However, there are four parts that seem to commonly be affected by pesticides: the frontal lobe, the temporal lobe, the limbic system, and the thalamus.
When the frontal lobe is impacted from the seizure, there can be negative impacts to the individual’s ability to make decisions, interact socially, and be attentive.
Temporal lobe damage could mean issues with visual perception, language, and hearing. On the other hand, limbic system damage, such as in the amygdala, relates to emotional and more behavioral problems.
Lastly, thalamus damage, alongside possible hippocampus damage, can negatively affect memory, sensory relay, and consciousness.
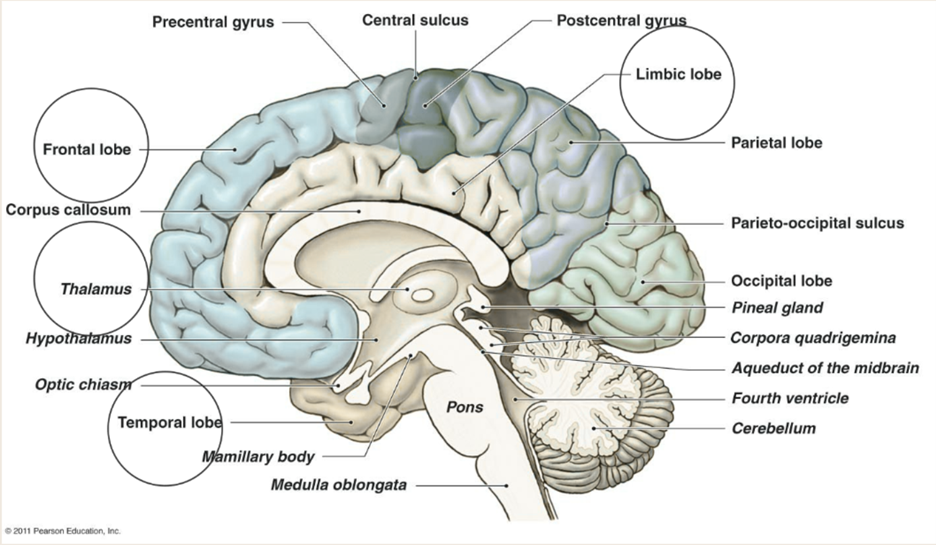
Figure 1 The temporal lobes, hippocampus, amygdala, frontal cortex, thalamus, and other limbic structures are the m.ain areas affected by pesticide-induced epilepsy. These areas are circled in the figure.
Treatment
Depending on what mechanism the pesticide acted through to lead to seizures, there are different treatment options. For when there is GABA receptor inhibition or hyperstimulation of cholinergic receptors, decontamination, or the person stopping exposure, is often the best way. More serious cases may require surgery as with other severe cases of epilepsy. Benzodiazepines are a common drug against seizures, and those are most beneficial in cases with ion flow changes or GABA receptor inhibition. This is especially since benzodiazepines enhance GABA activity. Oximes are another option, and they can increase activity of acetylcholinesterase. Consequently, excess acetylcholine is broken down, and cholinergic receptors are not as overactive.
Extra Considerations
Given all the above information, it is easy to see that there are risks associated with pesticide exposure. One of the important things to understand in order to help lower the risks is where pesticide exposures occur. Commercially, pesticides are used on a much larger scale and for much larger fields when compared to backyard gardens. This widespread use means the pesticide exposure levels are higher as well, leading to more risk for seizures or other health complications. Most recently, in 2023, there was a paper going further into what the ethical or social implications of this issue are, such as with who is under occupational exposure to pesticides, and it defines pesticides as a risk factor for epilepsy (Alarcon et al., 2023). Agricultural field workers may be from a low-income area as well, making it harder to properly care for serious medical conditions that they may have.
Most exposure to pesticides comes from agricultural areas, and the exposure can be through the air, water, or land. Once pesticides are in the environment, and being continually added, they may take years to completely degrade.
Conclusion
Pesticides and epilepsy are worth studying in conjunction. The four main mechanisms of pesticides leading to seizures involve lowering of GABA signaling, hyperstimulation of cholinergic receptors, increasing availability of acetylcholine, and changing ion flow in voltage-gated sodium channels.
Overall, benzodiazepines and oximes are the chemical treatment methods, while limiting exposure and undergoing surgery involve a variety of other methods, both medical and nonmedical.
The importance of this topic lies in how future research can be conducted to see how changing pesticide exposures impact individuals of different populations globally.
Author’s Bio
Sriya Reddy Gundlapally is an undergraduate student graduating in Fall 2025 from The University of Texas at Dallas with a B.S. degree in Biology and a minor in Public Health. Her topics of interest include the environment, human health, and community health.References
Jett, D. A. (2012). Chemical toxins that cause seizures. Neurotoxicology, 33(6), 1473-1475.
Requena, M., Parrón, T., Navarro, A., García, J., Ventura, M. I., Hernández, A. F., & Alarcón, R. (2018). Association between environmental exposure to pesticides and epilepsy. Neurotoxicology, 68, 13-18.
Alarcón, R., Giménez, B., Hernández, A. F., López-Villén, A., Parrón, T., García-González, J., & Requena, M. (2023). Occupational exposure to pesticides as a potential risk factor for epilepsy. Neurotoxicology, 96, 166-173.
Massachusetts General Hospital / MAPP. (n.d.). Your brain: An introduction to its anatomy. https://mapp.mgh.harvard.edu/your-brain-an-introduction-to-its-anatomy/