- Nov 18, 2025
Stroke -The Brain's Most Urgent Emergency
- Faisal Jahangiri
- ionm, neurophysiology, aphasia, Blogs, speech
- 0 comments
Silent But Deadly – What Happens When the Brain’s Circulation Fails
A stroke is one of the most sudden and often devastating events that can occur in the human body. Globally, stroke is the fifth leading cause of death, as well as a major cause of chronic disability (American Stroke Association, 2024).
A stroke occurs when there is a significant disruption in blood flow to a part of the brain. This can be due to a blockage or rupture of a blood vessel. Within minutes of the disruption, neurons begin to die, along with the body functions they control.
The brain, while accounting for only 2% of body weight, is incredibly oxygen hungry, consuming about 20% of the body’s oxygen (Raichle & Gusnard, 2002). During a stroke, when the blood supply is disrupted, neurons in the brain do not receive the oxygen that they need to generate energy, ultimately causing them to die.
There are various types of strokes, depending on whether there is a rupture or a blockage, as well as the location of the stroke.
Ischemic stroke is the most common stroke, accounting for about 87% of cases (American Stroke Association, 2024). This is when there is a blockage in the blood vessels. The blockage can be due to either a thrombus (thrombotic stroke) or an embolism (embolic stroke).
A thrombotic stroke occurs when fatty deposits cause a narrowing in the blood vessel over time, eventually causing a clot to form, resulting a blockage. An embolic stroke occurs when a blood clot forms elsewhere in the body, and then travels in the blood vessel, eventually reaching the brain and getting stuck, causing a blockage.
A hemorrhagic stroke accounts for the remaining 13% of stroke cases (American Stroke Association, 2024). This is when a blood vessel ruptures (bursts), leading to bleeding in the brain. Intracerebral hemorrhage is when the bleed is within the cortex. Subarachnoid or epidural hemorrhage is when the bleed is between the brain and its coverings (meninges).
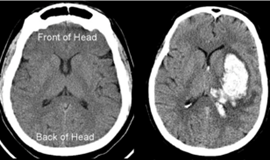
Figure 1. The right image shows a normal CT scan of the brain. The left image shows an intracerebral hemorrhagic stroke on the [patient’s] left hemisphere. This can be seen in the bright white spot, which is the blood from the ruptured blood vessel.
Every Minute Matters – You must act F.A.S.T.!
Stroke symptoms can strike suddenly and without warning. Knowing how to recognize them and act quickly can save a life. One of the most effective tools for remembering what to look for is the acronym F.A.S.T., recommended by the National Heart, Lung, and Blood Institute (2023).
F – Face Drooping
Check for unevenness in the face. Ask the person to smile. Does one side droop? Look closely at their eyes, cheeks, and lips for signs of asymmetry.
A – Arm Weakness
Ask them to raise both arms. Is one arm drifting downward or unable to lift? Sudden weakness or numbness in one arm is a red flag.
S – Speech Difficulty
Listen for slurred, garbled, or incoherent speech. Can they speak clearly and make sense? Trouble speaking or understanding language may signal a stroke.
T – Time to Call 911
If you notice any of these symptoms, even just one, call emergency services immediately. Let them know you suspect a stroke. Every minute matters when it comes to preserving brain function.
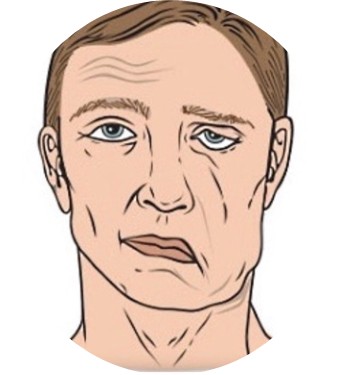
Figure 2. The illustration above depicts what a facial droop looks like, in this case, on the left side of the patient's face. Notice the drastic asymmetry of the face.
Who Is At Risk? – Prevention starts with knowing your risk
Risk builds up over time, and the more risk factors an individual has, the more likely it is that they will experience a stroke. Understanding your risk factors is the first major step towards stroke prevention.
Stroke risk is defined as the likelihood of an individual having a stroke based off a combination of factors. Some of these factors can change and are referred to as modifiable risk factors, while other factors cannot be changed.
Unchangeable risk factors include genetics, age, gender, and race (The Stroke Foundation, 2020). Family history and genetics play a major role; having a history of prior stroke also increases the risk for stroke substantially. After the age of 65, the risk of stroke increases. Gender also plays a role; women are at higher risk for stroke than men. Race also plays a role; African Americans, Hispanics, and Native Americans are more likely to have a stroke as they are at a higher risk for vascular disorders.
Modifiable risk factors are typically reflective of lifestyle choices. Eating a balanced diet and regular exercise are incredibly important in terms of lowering the risk of stroke. Both lifestyle factors lower the chances of hypertension, high cholesterol, diabetes, obesity, and other vascular diseases, furthering reducing the risk of stroke (The Stroke Foundation, 2020).
Regularly smoking and drinking can have major impacts in increasing your risk for stroke as they cause hypertension and can even cause damage to your blood vessels (The Stroke Foundation, 2020). Chronic sedentary lifestyles can enable poor lifestyle choices, thus increasing the risk for stroke.
All modifiable risk factors are preventable and/or treatable (The Stroke Foundation, 2020). When it comes to stroke, prevention is key. That is why it is so important to know your risk factors, and then to evaluate the lifestyle changes you need in order to reduce your risk for stroke.

Figure 3. High blood pressure (hypertension) is one of the leading modifiable risk factors for stroke. Age, obesity, and poor diet and exercise all contribute to increased risk of hypertension, and thus contribute to a higher risk of stroke (The Stroke Foundation, 2020).
Strokes in young people - Why are people having strokes before their 50s?
In 2023, the University of California Health (UCHealth) reported that “the number of young adults having strokes in northern Colorado has nearly doubled over the last few years” (Blocker & UCHealth, 2023). This reflects a nationwide trend: the number of strokes among people aged 18-45 has been increasing faster than in any other age group over the past few years (Blocker & UCHealth, 2023). The question is, why?
At first, strokes in younger populations were typically due to unmodifiable risk factors, but now, it’s becoming apparent how quickly poor lifestyle choices can significantly heighten stroke risk.
Unhealthy eating (especially with the affordability and convenience of fast food in the United States) and being obese and overweight have become more and more common and normalized, contributing to a higher risk of stroke. Drinking alcohol, smoking, and using drugs are activities that often start at younger ages, further increasing the risk of stroke at a younger age (Blocker & UCHealth, 2023). UCHealth also speculates on the relationship between COVID-19 and “sticky blood,” in which blood becomes abnormally thick and more prone to clotting after exposure to the virus (Blocker & UCHealth, 2023).
Overall, this emerging trend in the increase of strokes amongst younger individuals is a huge wake-up call to the impacts of modifiable risk factors for strokes, and further highlights that prevention is key.
How Does Diagnosis Work? Finding answers fast
A diagnosis of stroke details what type of stroke occurred, what caused the stroke, what part(s) of the brain and body were affected, and whether there is bleeding in the brain (National Heart, Lung, and Blood Institute, 2023). The diagnosis is made by the doctor by piecing together the patient’s history, presenting symptoms, physical exam, and test results (National Heart, Lung, and Blood Institute, 2023).
When a stroke is first suspected and the patient is in the emergency room, a CT scan of the brain is done to differentiate between a hemorrhagic and ischemic stroke. An MRI (a more detailed scan) may also be performed to better assess the brain areas affected. Blood tests will assess your blood cell count and glucose levels to ensure they are stable (National Heart, Lung, and Blood Institute, 2023). This also helps determine which medication to administer. The doctor will ask you about your risk factors for stroke, as well as your signs and symptoms when they began. The doctor will also conduct a physical exam, during which they will assess mental alertness, balance and coordination, numbness or weakness in the face or extremities, and speech and diction (National Heart, Lung, and Blood Institute, 2023). This information is key to determining the best treatment and recovery.
Stroke Treatment & Recovery – What happens next?
Timing is crucial in stroke treatment. That is why it is critical that someone provide a timeline of symptom onset and progression. As mentioned in the previous section, one of the first things that will be done in the emergency room for a stroke is a CT scan, and this will determine if the stroke is hemorrhagic or ischemic. Then treatment begins.
For ischemic stroke, treatment is relatively straightforward as it is centered around one goal: find the blockage and remove it. The first line of treatment is tissue plasminogen activator (tPA), which must be administered within three (3) hours of the onset of stroke symptoms (National Heart, Lung, and Blood Institute, 2023). If it is after three hours, a blood-thinning or anti-clotting medication will be given (National Heart, Lung, and Blood Institute, 2023). This is to prevent more clots from forming or from getting bigger. The last line of treatment is a thrombectomy (National Heart, Lung, and Blood Institute, 2023). This is when a thin tube is inserted into your blood vessels (typically in your thigh, since the vessels are larger there) and travels to the blockage. Inside the tube is a stent retriever, which essentially grabs and removes the clot causing the stroke. Another procedure may also be suggested depending on the specific cause of the stroke and the extent of the brain damage (National Heart, Lung, and Blood Institute, 2023).
A hemorrhagic stroke can be a bit more challenging to treat as it is caused when a blood vessel ruptures. There are many things that need to be managed: blood pressure needs to be lowered to slow bleeding, and clotting needs to be promoted to close the rupture (Cleveland Clinic, 2022). If the pressure in the brain from the high volume of leaked blood is too high, emergency surgery may be needed to relieve it (Cleveland Clinic, 2022).
Recovery from stroke looks different for everyone. Rehabilitation is essential to maximize recovery and minimize lasting deficits from the stroke. While the neurons that die in stroke cannot regenerate, stroke recovery and rehabilitation are based on the concept of neuroplasticity. Neuroplasticity is the brain’s ability to rewire and organize its connections and circuits, and this reorganization enables recovery of lost functions. For the brain to know it needs to reorganize its circuits, it requires regular stimulation, which is provided through various therapies. For example, if after a stroke a patient has difficulty moving their right arm, they need to attend regular physical therapy, where they consistently perform various exercises with their right arm, as this stimulates and signals the brain to begin the slow process of rewiring and recovery.

Figure 4. Rehabilitation and therapy are very crucial for post-stroke recovery!
Stem Cell Therapy – Stanford clinical trial results
In late 2016, the Stanford University School of Medicine published findings from a small clinical trial of patients with motor deficits due to stroke (Goldman, 2016). This study focused on mesenchymal stem cells and their ability to differentiate into various cell types.
For the trial, modified mesenchymal stem cells were injected directly into the brain, specifically into the areas surrounding the stroke-damaged tissue. Although the mesenchymal cells did not survive long in the brain, their effects persisted beyond their lifespan (Goldman, 2016). Within a month, patients showed significant motor recovery, with continued improvement for months and, in some cases, even years afterward (Goldman, 2016). Dr. Gary Steinberg, the lead investigator of the study, noted that although the primary purpose of the trial was to assess the procedure's safety, the improvement in motor function was both statistically significant and clinically meaningful (Goldman, 2016). He stated, “This could revolutionize our concept of what happens after not only stroke but also traumatic brain injury and even neurodegenerative disorders” (Goldman, 2016).
It is important to note that stem cell therapy remains a novel concept and is not currently FDA-approved in the United States. However, countries like Germany and Switzerland are at the forefront of stem cell therapy and have incorporated these treatments into their clinical care.
Although clinical stem cell therapy is still under extensive research, this small study demonstrated how it could be the difference between a patient being confined to a wheelchair and regaining the ability to walk. Stem cell therapy has the potential to revolutionize healthcare and recovery, extending beyond the nervous system.
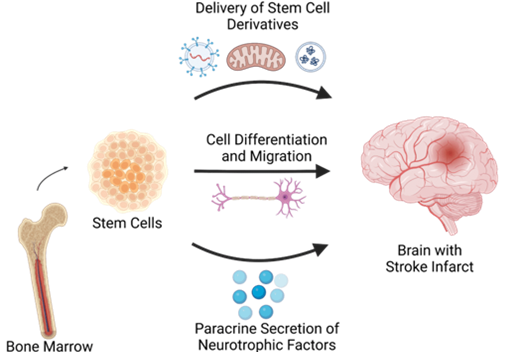
Figure 5. The above diagram illustrates the three mechanisms by which stem cells can help repair brain injuries. They can release helpful cellular components (such as mitochondria and vesicles) that aid healing. They can differentiate (turn into) new brain cells that help in making new connections. They can release neurotrophic factors (growth factors) that help existing neurons thrive and form new connections. (Colliander et al., 2023).
Conclusion: Key takeaways
Stroke is a medical emergency, and it is critical to act F.A.S.T. to minimize the damage. There are two main types of strokes: ischemic (about 87% of cases) and hemorrhagic (about 13% of cases). Ischemic stroke occurs when there is a blockage in a blood vessel, either due to a thrombus (an obstruction that forms at the site of blockage) or an embolism (the obstruction travels from another part of the body and gets stuck in a blood vessel in the brain). A hemorrhagic stroke occurs when a blood vessel ruptures and leaks blood into the brain. Both types of stroke result in neuronal cell death.
It is important to know your risk factors for stroke to prevent stroke. There are unchangeable risk factors such as aging, genetics, family and stroke history, gender, and race. Then there are modifiable (changeable) risk factors that typically have to do with lifestyle choices, such as drugs, alcohol, diet, exercise, and vascular health.
Stroke diagnosis involves evaluating patient history, symptom onset and timeline, physical exam, and imaging and test results. This then explains the cause of the stroke, steps for treatment, and the type of medication to administer. The deficits post-stroke determine the type of therapies required to minimize them and regain as much functionality as possible. Recovery looks different for every patient.
R E F E R E N C E S
American Stroke Association. (2024). About Stroke. American Stroke Association. https://www.stroke.org/en/about-stroke
Blocker, K., & UCHealth. (2023, November 6). Strokes in young people: They’re occurring more often. Why? UCHealth Today. https://www.uchealth.org/today/why-are-strokes-in-young-people-occurring-more-often/
Cleveland Clinic. (2022). Hemorrhagic Stroke: What It Is, Causes, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23969-hemorrhagic-stroke
Colliander, R., Alleman, K., Diaz, M., Jimenez, M., King, P., Mirpuri, P., Cutler, C., & Lucke-Wold, B. (2023). Stem Cell Implants: Emerging Innovation for Stroke Recovery. Journal of Neuro and Oncology Research. https://athenaeumpub.com/wp-content/uploads/Stem-Cell-Implants-Emerging-Innovation-for-Stroke-Recovery.pdf
Goldman, B. (2016, June 2). Stem cells shown safe, beneficial for chronic stroke patients. News Center. https://med.stanford.edu/news/all-news/2016/06/stem-cells-shown-safe-beneficial-for-chronic-stroke-patients.html
National Heart, Lung and Blood Institute. (2023, May 26). Stroke - What Is a Stroke? Www.nhlbi.nih.gov. https://www.nhlbi.nih.gov/health/stroke
Raichle, M. E., & Gusnard, D. A. (2002). Appraising the brain’s energy budget. Proceedings of the National Academy of Sciences, 99(16), 10237–10239. https://doi.org/10.1073/pnas.172399499
The Stroke Foundation. (2020). Stroke Warning Signs – The Stroke Foundation. Thestrokefoundation.org. https://www.thestrokefoundation.org/stroke-facts/stroke-warning-signs